
Medication side effects: What are your options?

Medications can provide a host of health benefits. They may prevent or eliminate a disease. They might improve your quality of life and even help you live longer. But the medicines we take also have potential side effects. While listed side effects don’t always occur, it’s always possible.
And though that’s unfortunate, it also makes sense: while fighting the good fight against infection, cancer, or other health issues, medicines can also affect normal, healthy parts of the body. That can lead to bothersome symptoms and, sometimes, deadly consequences.
What are the most common and annoying side effects?
If you think you’re experiencing a medication side effect, you can check the National Library of Medicine database for the medicines you take to learn about their side effects.
Among the most common side effects caused by medicines are:
- nausea, constipation, diarrhea
- dry mouth
- drowsiness
- rash
- headache.
While the nature and severity of drug side effects vary widely, some are more bothersome than others. For example, sexual side effects can be especially distressing (and are likely underreported). And forgetfulness or trouble concentrating (often called “brain fog”) can have a serious impact on daily functioning, employment, and quality of life.
Which medication side effects are dangerous?
Though most side effects from medicines are more bothersome than dangerous, there are exceptions. Here are four serious drug side effects that require immediate medical attention.
- Anaphylaxis. This is a sudden allergic reaction affecting many parts of the body, including rash; swelling of the lips, tongue, or throat; and trouble breathing.
- Stevens-Johnson Syndrome (SJS) and toxic epidermal necrolysis (TEN). These two related allergic conditions are marked by severe, widespread rash, skin peeling, and fever. The main difference between them is that skin damage is more severe in TEN. Complications can be life-threatening, such as kidney and lung injury, or skin detachment similar to experiencing a serious burn.
- Drug reaction with eosinophilia and systemic symptoms (DRESS). This rare reaction to medications causes abnormal blood counts, rash, enlarged lymph nodes, and liver injury. Other organs, including the kidneys, lungs, and heart, may be harmed.
What about drug interactions?
Some medicines may cause no side effects until you start taking a second one. That’s because drugs can interact — that is, one drug alters the effects of another drug.
For example, if you take a blood thinner, also taking an anti-inflammatory medicine like ibuprofen or naproxen can suddenly increase your risk of bleeding.
There are thousands of known drug interactions. Medication prescribers, pharmacists, and computerized prescription ordering systems routinely check for them in advance so they can be avoided.
Are medication side effects ever a good thing?
Yes, indeed. In fact, some drugs developed to treat one condition have been approved for something entirely different because of what might be called positive side effects.
That’s how a blood pressure medicine (minoxidil) became a blockbuster treatment for hair loss (Rogaine and other brands). Another medicine (sildenafil), also developed for high blood pressure, was found to trigger erections in men. This lead to its approval as Viagra. There are many other examples of the good side of side effects.
When should you contact your health care provider?
If you suspect you’re experiencing a medication side effect, let your health care provider know. They can help you make the choice that’s best for you.
For serious or dangerous side effects like the examples noted above, it’s important to stop the drug and seek treatment right away. Let the FDA know as well. The FDA welcomes voluntary reporting of serious side effects so they can learn more about a drug’s impact on users, and take steps to improve its safety if necessary. Improvements might include new medication labeling, or even a recall.
For less serious side effects your first inclination might also be to stop the drug. But that’s not always the best choice. While stopping the drug may eliminate the side effect, you’ll also lose the drug’s benefit.
Here are some options your health care provider may suggest:
- Wait. If the side effect is minor, you could decide to put up with it to see if it goes away on its own as your body adjusts to the medication. If time doesn’t help, you may need to decide with your doctor whether the benefits of the medicine outweigh the side effects.
- Reduce. Your health care provider may suggest reducing the dose or how often you take the drug, which may improve or eliminate the side effects.
- Stop. You and your health care provider could decide to stop the medicine and consider a different treatment option, or reconsider whether treatment is still necessary.
- Add. Sometimes it’s reasonable to take a second drug to treat the first drug’s side effects. This option is not ideal. Taking a second drug to treat side effects from the first drug adds yet another medicine to your list. And that second drug could cause its own side effects, or even prompt the need to repeat this sequence with more medications. But sometimes adding another medication is a good option. For example, it’s reasonable to take an over-the-counter medicine (such as acetaminophen or ibuprofen) to treat a mild drug side effect (such as headache). Or if a medicine that causes a significant side effect is actually working well for a serious health condition, then adding a second medicine might make sense.
The bottom line
Drug developers may someday discover the perfect medicine, one that provides major health benefits without any risk of side effects. Until that happens, though, there are many ways to handle drug side effects. The challenge is figuring out which one is best for you.
About the Author
Robert H. Shmerling, MD, Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Robert H. Shmerling is the former clinical chief of the division of rheumatology at Beth Israel Deaconess Medical Center (BIDMC), and is a current member of the corresponding faculty in medicine at Harvard Medical School. … See Full Bio View all posts by Robert H. Shmerling, MD
Court ruling curbs unfounded claims for memory supplement
I must have seen commercials for Prevagen 50 times: story after story from everyday people who describe improvement in memory once they began taking Prevagen. And perhaps you recall older commercials playing off the idea that many people take supplements that boast of gut, joint, and heart health claims. Those commercials memorably asked, “So why wouldn’t you take something for the most important part of you… your brain? With an ingredient originally found in jellyfish! Healthier brain, better life!”
Never mind that the ingredient from jellyfish (apoaequorin) that was supposed to deliver these benefits has no known role in human memory. Or that many experts believe supplements like this are most likely digested in the stomach and never wind up anywhere near the brain.
Can a supplement actually improve memory? If it doesn’t work, why is the manufacturer allowed to suggest it does? And if apoaequorin is so great, why aren’t jellyfish smarter (as a colleague of mine wonders)?
Mind the gap between graphics and reality
A bar graph in the older ads showed a rise from 5% to 10% to 20% over 90 days in “recall tasks,” though exactly what that meant was never explained. Nor were we told how many people were studied or given any information about effects on memory after 90 days.
One small, company-sponsored study reported improvements in memory after people took apoaequorin. However, the published version demonstrated improvements only in a subset of study participants. And the real-world impact of these changes is uncertain. The study authors recommended additional research to clarify its effectiveness. But I’ve been unable to find any additional, high-quality, independent studies showing the impact of Prevagen or apoaequorin on human memory.
The Prevagen case resolved
The US Federal Trade Commission (FTC) and the New York state attorney general were also unconvinced about the supplement’s benefits. Back in 2017, they charged the supplement maker with false advertising. Fast forward to February 2024, when a New York jury found that many of the supplement’s claims were not supported by reliable evidence, and some (but not all) of the claims were “materially misleading.”
In December 2024, the FTC and New York attorney general won their lawsuit. Now the makers of Prevagen are prohibited from claiming that the supplement can improve brain function or memory.
Supplement claims sound good — so why the disclaimers?
There are many thousands of supplements marketed for hundreds of conditions. But it’s often hard to say if they’re doing much of anything.
For example:
- Glucosamine is often promoted as good for joint health. I have known patients who swore by it. But the best studies suggest this supplement has modest effects, if any.
- When vitamins tout heart-healthy claims, I think of the example of vitamin E, once considered potentially useful to prevent or treat heart disease. Yet, study after study showed no benefit. In fact, it may increase the risk of heart failure.
- As for probiotic supplements, no convincing evidence shows that their use improves digestive health or prevents digestive disease in healthy people.
So when you’re considering supplements, be skeptical of the benefits touted and remember the standard disclaimer stamped on each one: “These statements have not been evaluated by the FDA.”
What are the rules?
Supplement makers are bound by a few basic rules set by the FTC and FDA:
- They can make truthful claims about connections between their supplement and the body’s “structure and function.” For example, a vitamin maker touting calcium in a product can say that calcium is important for bone health — although it’s also true that calcium supplements may offer little or nothing for most people with healthy bones, diets rich in calcium, and no medical condition requiring extra calcium.
- They cannot claim their product treats or prevents a particular disease. That disclaimer, which may seem to contradict marketing promises, must appear on every package. So, commercials suggesting that a supplement can reverse or slow Alzheimer’s disease, or any dementia, may run afoul of the rules on marketing supplements.
The FDA and FTC continue to provide key oversight to the dietary supplement industry. That’s a daunting task given the sheer volume of products on the market.
The bottom line
This country has an enormous appetite for dietary supplements. The supplement industry is now worth an estimated $70 billion or more, with as many as 100,000 products available for purchase.
But there’s a reason dietary supplements carry a disclaimer: “This product is not intended to diagnose, treat, cure, or prevent any disease.” This should remind us all to be wary of claims we see in ads for dietary supplements. Unlike prescription drugs, supplements are not thoroughly tested or evaluated. While dietary supplements might provide benefits in certain cases, it’s vitally important that their makers not make unfounded claims to exploit consumers.
I support the efforts of the FDA and FTC to regulate dietary supplements and their ads. But regardless of how effective their regulations are, it’s best to be skeptical about ads for products that seem too good to be true. There’s a good chance they are.
About the Author
Robert H. Shmerling, MD, Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Robert H. Shmerling is the former clinical chief of the division of rheumatology at Beth Israel Deaconess Medical Center (BIDMC), and is a current member of the corresponding faculty in medicine at Harvard Medical School. … See Full Bio View all posts by Robert H. Shmerling, MD
Let’s not call it cancer
Roughly one in six men will be diagnosed with prostate cancer at some point in their lives, but these cancers usually aren’t life-threatening. Most newly diagnosed men have Grade Group 1 (GG1) prostate cancer, which can linger for years without causing significant harms.
Prostate cancer is categorized according to how far it has spread and how aggressive it looks under the microscope. Pure GG1 prostate cancer is the least risky form of the disease. It occurs frequently with age, will not metastasize to other parts of the body, and it doesn’t require any immediate treatment.
So, should we even call it cancer? Many experts say no.
Dr. Matthew Cooperberg, who chairs the department of urology at the University of California, San Francisco, says men wouldn’t suffer as much anxiety — and would be less inclined to pursue unneeded therapies — if their doctors stopped referring to low-grade changes in the prostate as cancer. He recently co-chaired a symposium where experts from around the world gathered to discuss the pros and cons of giving GG1 cancer another name.
Treatment discrepancies
GG1 cancer is typically revealed by PSA screening. The goal with screening is to find more aggressive prostate cancer while it’s still curable, yet these efforts often detect GG1 cancer incidentally. Attendees at the symposium agreed that GG1 disease should be managed with active surveillance. With this standard practice, doctors monitor the disease with periodic PSA checks, biopsies, and imaging, and treat the disease only if it shows signs of progression.
But even as medical groups work to promote active surveillance, 40% of men with low-risk prostate cancer in the United States are treated immediately. According to Dr. Cooperberg, that’s in part because the word “cancer” has such a strong emotional impact. “It resonates with people as something that spreads and kills,” he says. “No matter how much we try to get the message out there that GG1 cancer is not an immediate concern, there’s a lot of anxiety associated with a ‘C-word’ diagnosis.”
A consequence is widespread overtreatment, with tens of thousands of men needlessly suffering side effects from surgery or radiation every year. A cancer diagnosis has other harmful consequences: studies reveal negative effects on relationships and employment as well as “someone’s ability to get life insurance,” Dr. Cooperberg says. “It can affect health insurance rates.”
Debate about renaming
Experts at the symposium proposed that GG1 cancer could be referred to instead as acinar neoplasm, which is an abnormal but nonlethal growth in tissue. Skeptics expressed a concern that patients might not stick with active surveillance if they aren’t told they have cancer. But should men be scared into complying with appropriate monitoring? Dr. Cooperberg argues that patients with pure GG1 “should not be burdened with a cancer diagnosis that has zero capacity to harm them.”
Dr. Cooperberg does caution that since biopsies can potentially miss higher-grade cancer elsewhere in the prostate, monitoring the condition with active surveillance is crucial. Moreover, men with a strong family history of cancer, or genetic mutations such as BRCA1 and BRCA2 that put them at a higher risk of aggressive disease, should be followed more closely, he says.
Dr. Marc Garnick, the Gorman Brothers Professor of Medicine at Harvard Medical School and Beth Israel Deaconess Medical Center, and editor in chief of the Harvard Medical School Guide to Prostate Diseases, agrees. Dr. Garnick emphasized that a name change for GG1 cancer needs to consider a wide spectrum of additional testing. “This decision can’t simply be based on pathology,” he says. “Biopsies only sample a miniscule portion of the prostate gland. Genetic and genomic tests can help us identify some low-risk cancers that might behave in a more aggressive fashion down the road.”
Meanwhile, support for a name change is gaining momentum. “Younger pathologists and urologists are especially likely to think this is a good idea,” Dr. Cooperberg says. “I think the name change is just a matter of time — in my view, we’ll get there eventually.”
About the Author

Charlie Schmidt, Editor, Harvard Medical School Annual Report on Prostate Diseases
Charlie Schmidt is an award-winning freelance science writer based in Portland, Maine. In addition to writing for Harvard Health Publishing, Charlie has written for Science magazine, the Journal of the National Cancer Institute, Environmental Health Perspectives, … See Full Bio View all posts by Charlie Schmidt
About the Reviewer
Marc B. Garnick, MD, Editor in Chief, Harvard Medical School Annual Report on Prostate Diseases; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Marc B. Garnick is an internationally renowned expert in medical oncology and urologic cancer. A clinical professor of medicine at Harvard Medical School, he also maintains an active clinical practice at Beth Israel Deaconess Medical … See Full Bio View all posts by Marc B. Garnick, MD

Why all the buzz about inflammation — and just how bad is it?

Quick health quiz: how bad is inflammation for your body?
You’re forgiven if you think inflammation is very bad. News sources everywhere will tell you it contributes to the top causes of death worldwide. Heart disease, stroke, dementia, and cancer all have been linked to chronic inflammation. And that’s just the short list. So, what can you do to reduce inflammation in your body?
Good question! Before we get to the answers, though, let’s review what inflammation is — and isn’t.
Inflammation 101
Misconceptions abound about inflammation. One standard definition describes inflammation as the body’s response to an injury, allergy, or infection, causing redness, warmth, pain, swelling, and limitation of function. That’s right if we’re talking about a splinter in your finger, bacterial pneumonia, or the rash of poison ivy. But it’s only part of the story, because there’s more than one type of inflammation:
- Acute inflammation rears up suddenly, lasts days to weeks, and then settles down once the cause, such as an injury or infection, is under control. Generally, acute inflammation is a reaction that attempts to restore the health of the affected area. That’s the type described in the definition above.
- Chronic inflammation is quite different. It can develop for no medically apparent reason, last a lifetime, and cause harm rather than healing. This type of inflammation is often linked with chronic disease, such as:
-
- excess weight
- diabetes
- cardiovascular disease, including heart attacks and stroke
- certain infections, such as hepatitis C
- autoimmune disease
- cancer
- stress, whether psychological or physical.
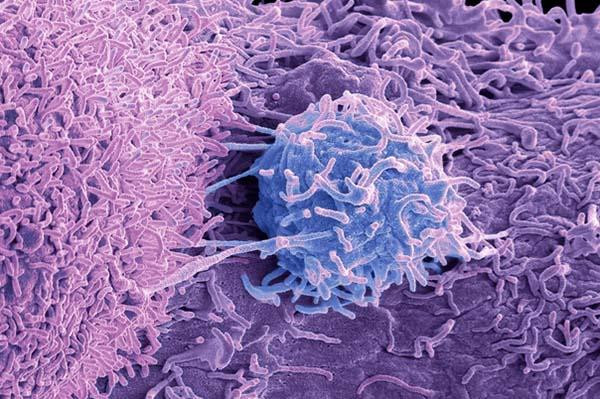
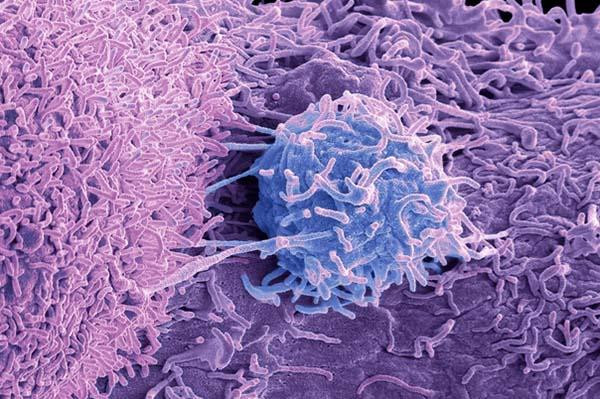
Which cells are involved in inflammation?
The cells involved with both types of inflammation are part of the body’s immune system. That makes sense, because the immune system defends the body from attacks of all kinds.
Depending on the duration, location, and cause of trouble, a variety of immune cells, such as neutrophils, lymphocytes, and macrophages, rush in to create inflammation. Each type of cell has its own particular role to play, including attacking foreign invaders, creating antibodies, and removing dead cells.
4 inflammation myths and misconceptions
Inflammation is the root cause of most modern illness.
Not so fast. Yes, a number of chronic diseases are accompanied by inflammation. In many cases, controlling that inflammation is an important part of treatment. And it’s true that unchecked inflammation contributes to long-term health problems.
But inflammation is not the direct cause of most chronic diseases. For example, blood vessel inflammation occurs with atherosclerosis. Yet we don’t know whether chronic inflammation caused this, or whether the key contributors were standard risk factors (such as high cholesterol, diabetes, and smoking — all of which cause inflammation).
You know when you’re inflamed.
True for some conditions. People with rheumatoid arthritis, for example, know when their joints are inflamed because they experience more pain, swelling, and stiffness. But the type of inflammation seen in obesity, diabetes, or cardiovascular disease, for example, causes no specific symptoms. Sure, fatigue, brain fog, headaches, and other symptoms are sometimes attributed to inflammation. But plenty of people have those symptoms without inflammation.
Controlling chronic inflammation would eliminate most chronic disease.
Not so. Effective treatments typically target the cause of inflammation, rather than just suppressing inflammation itself. For example, a person with rheumatoid arthritis may take steroids or other anti-inflammatory medicines to reduce their symptoms. But to avoid permanent joint damage, they also take a medicine like methotrexate to treat the underlying condition that’s causing inflammation.
Anti-inflammatory diets or certain foods (blueberries! kale! garlic!) prevent disease by suppressing inflammation.
While it’s true that some foods and diets are healthier than others, it’s not clear their benefits are due to reducing inflammation. Switching from a typical Western diet to an “anti-inflammatory diet” (such as the Mediterranean diet) improves health in multiple ways. Reducing inflammation is just one of many possible mechanisms.
The bottom line
Inflammation isn’t a lone villain cutting short millions of lives each year. The truth is, even if you could completely eliminate inflammation — sorry, not possible — you wouldn’t want to. Among other problems, quashing inflammation would leave you unable to mount an effective response to infections, allergens, toxins or injuries.
Inflammation is complicated. Acute inflammation is your body’s natural, usually helpful response to injury, infection, or other dangers. But it sometimes sparks problems of its own or spins out of control. We need to better understand what causes inflammation and what prompts it to become chronic. Then we can treat an underlying cause, instead of assigning the blame for every illness to inflammation or hoping that eating individual foods will reduce it.
There’s no quick or simple fix for unhealthy inflammation. To reduce it, we need to detect, prevent, and treat its underlying causes. Yet there is good news. Most often, inflammation exists in your body for good reason and does what it’s supposed to do. And when it is causing trouble, you can take steps to improve the situation.
About the Author
Robert H. Shmerling, MD, Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Robert H. Shmerling is the former clinical chief of the division of rheumatology at Beth Israel Deaconess Medical Center (BIDMC), and is a current member of the corresponding faculty in medicine at Harvard Medical School. … See Full Bio View all posts by Robert H. Shmerling, MD